Raw foodism from Wikipedia
Enzymes from Wikipedia
Do you ever wonder what you really know about Crohn's Disease despite your experience and all the information out there? Do you find yourself unsettled, wondering why the pieces never seem to really fit together? Through simple questions linked to research evidence, this blog is a place where you can think quietly about Crohn's Disease, its cause, nature, and control. Join me in constructing a new view of Crohn's Disease. Your comments are gold.
Showing posts with label diet. Show all posts
Showing posts with label diet. Show all posts
16.4.12
25.1.12
Would a Nutrigenomic Diet reduce Crohn's symptoms?
"Nutrigenomics in the whole-genome scanning era: Crohn’s disease as example" in Cellular and Molecular Science (2007)
"Nutrigenomics has the potential to tailor diets to optimize health, based on knowledge of key genetic polymorphisms. Identification of candidate genes is often based on a priori knowledge of disease processes. However, genome-wide association methods are not only validating previously identified genes and polymorphisms, but also revealing new gene-disease associations not anticipated from prior knowledge. In Crohn’s disease (CD), such studies not only confirm the importance of caspase-activated recruitment domain 15 and major histocompatability complex II molecules, but also reveal strong associations with the proinflammatory cytokine interleukin-23 receptor and autophagy-related 16-like gene. Genes identified to date in CD can be linked into two interrelated pathways: receptor-mediated cytokine induction or autophagocytosis. New genomic technologies need to be matched with innovative methodologies to characterize the likely impact of foods and to take the field to another dimension of value for human diet development and optimized health."
"Nutrigenomics has the potential to tailor diets to optimize health, based on knowledge of key genetic polymorphisms. Identification of candidate genes is often based on a priori knowledge of disease processes. However, genome-wide association methods are not only validating previously identified genes and polymorphisms, but also revealing new gene-disease associations not anticipated from prior knowledge. In Crohn’s disease (CD), such studies not only confirm the importance of caspase-activated recruitment domain 15 and major histocompatability complex II molecules, but also reveal strong associations with the proinflammatory cytokine interleukin-23 receptor and autophagy-related 16-like gene. Genes identified to date in CD can be linked into two interrelated pathways: receptor-mediated cytokine induction or autophagocytosis. New genomic technologies need to be matched with innovative methodologies to characterize the likely impact of foods and to take the field to another dimension of value for human diet development and optimized health."
23.1.12
Does school cafeteria food trigger Crohn's?
healthy school lunches
school cafeteria
kids school lunches
high school cafeteria food
good school lunches
healthy school lunches for kids
cafeteria food in schools
"School Food Environments and Practices Affect Dietary Behaviors of US Public School Children" in Journal of the American Dietetic Association (2009)
"To improve children's diet and reduce obesity continued changes to school food environments and practices are essential. Removing sugar-sweetened beverages from school food stores and snack bars, improving à la carte choices, and reducing the frequency of offering french fries merit testing as strategies to reduce energy from low-nutrient, energy-dense foods at school."
Free for all: fixing school food in America by Janet Poppendieck
"What about the toxic burden from pesticides and fertilizers used in the production of the preponderance of fruits and vegetables served in schools that are not organically grown? What about the hormones in the milk and meat? What about the unknown consequences of ingesting modeified organisms (GMOs)?" (p. 132)
Lunch Wars: How to Start a School Food Revolution and Win the Battle for Our Children's Health,
Amy Kalafa (2011) [preview with no page numbers]
"I hadn't actually been in a public school lunchroom in years, so one of the first places I filmed was my daughter-s middle school cafeteria. Reading the labels on the many packaged products for sale confirmed my worst suspicons: the school cfeteria was a microcosm of American fake food culture. Healthy-sounding products like Nutri-Grain bars had high fructose corn syrup listed as one of the first ingredients (well hidden under a foil flap that you had to fold down to read the tiny print!). The low-fat yogurt also had high fructose corn syrup, aspartame (artifical sweetener), artificial flavoring, and coloring. ... I was truly shocked to discover that she had been purchasing fries, Rice Krispies Treats, Pop-Tarts, and soft drinks on a daily basis."
"For years, I lived in denial, thinking that my kids were immune to all the advertising and promotion because we ate well at home. When I went to the middle school cafeteria to film there and learned that my daughter had been eating junk food nearly every day, I realized that the school was actually encouraging this behavior, making junk food socially acceptable. Although they were teaching so-called proper nutrition in health class, the message in the cafeteria was 'anything goes'. A conversation with the school's then-superintendent confirmed that indeed, he found no contradiction in the messaging because, he insisted, it was not the school district's responsibility to feed the kids, just to educate them."
"Case Study: Aphthous Ulcers in a 14-Year-Old Girl" in Continuing Nursing Education (2011)
"Briana is unable to associate any particular foods with abdominal discomfort or diarrhea. She usually enjoys a varied diet. She has not been treated with antibiotics in the past year. Her mother denies any foreign travel. The family usually eats at a restaurant once every 2 weeks, and Briana eats lunch prepared by the school cafeteria." [Italics mind.]
school cafeteria
kids school lunches
high school cafeteria food
good school lunches
healthy school lunches for kids
cafeteria food in schools
"School Food Environments and Practices Affect Dietary Behaviors of US Public School Children" in Journal of the American Dietetic Association (2009)
"To improve children's diet and reduce obesity continued changes to school food environments and practices are essential. Removing sugar-sweetened beverages from school food stores and snack bars, improving à la carte choices, and reducing the frequency of offering french fries merit testing as strategies to reduce energy from low-nutrient, energy-dense foods at school."
Free for all: fixing school food in America by Janet Poppendieck
"What about the toxic burden from pesticides and fertilizers used in the production of the preponderance of fruits and vegetables served in schools that are not organically grown? What about the hormones in the milk and meat? What about the unknown consequences of ingesting modeified organisms (GMOs)?" (p. 132)
Lunch Wars: How to Start a School Food Revolution and Win the Battle for Our Children's Health,
Amy Kalafa (2011) [preview with no page numbers]
"I hadn't actually been in a public school lunchroom in years, so one of the first places I filmed was my daughter-s middle school cafeteria. Reading the labels on the many packaged products for sale confirmed my worst suspicons: the school cfeteria was a microcosm of American fake food culture. Healthy-sounding products like Nutri-Grain bars had high fructose corn syrup listed as one of the first ingredients (well hidden under a foil flap that you had to fold down to read the tiny print!). The low-fat yogurt also had high fructose corn syrup, aspartame (artifical sweetener), artificial flavoring, and coloring. ... I was truly shocked to discover that she had been purchasing fries, Rice Krispies Treats, Pop-Tarts, and soft drinks on a daily basis."
"For years, I lived in denial, thinking that my kids were immune to all the advertising and promotion because we ate well at home. When I went to the middle school cafeteria to film there and learned that my daughter had been eating junk food nearly every day, I realized that the school was actually encouraging this behavior, making junk food socially acceptable. Although they were teaching so-called proper nutrition in health class, the message in the cafeteria was 'anything goes'. A conversation with the school's then-superintendent confirmed that indeed, he found no contradiction in the messaging because, he insisted, it was not the school district's responsibility to feed the kids, just to educate them."
"Case Study: Aphthous Ulcers in a 14-Year-Old Girl" in Continuing Nursing Education (2011)
"Briana is unable to associate any particular foods with abdominal discomfort or diarrhea. She usually enjoys a varied diet. She has not been treated with antibiotics in the past year. Her mother denies any foreign travel. The family usually eats at a restaurant once every 2 weeks, and Briana eats lunch prepared by the school cafeteria." [Italics mind.]
9.11.11
Does an offal-rich diet influence Crohn's?
22.7.11
22.6.11
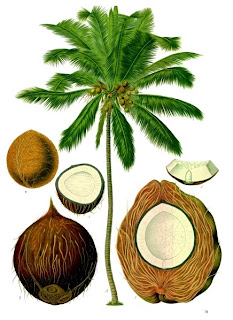
Does eating coconut oil and other medium-chain triglycerides (MCTs) reduce Crohn's symptoms?
"Coconut Oil and Medium-Chain Triglycerides" from Coconut Research Center
"MCTs passively diffuse from the GI tract to the portal system (longer fatty acids are absorbed into the lymphatic system) without requirement for modification like long-chain fatty acids or very-long-chain fatty acids. In addition, MCTs do not require bile salts for digestion. Patients that have malnutrition or malabsorption syndromes are treated with MCTs because they do not require energy for absorption, utilization, or storage. Coconut oil is composed of approximately 66% medium-chain triglycerides. Other rich sources of MCTs include palm kernel oils and camphor tree drupes. The fatty acids found in MCTs are called medium-chain fatty acids. The names of the medium-chain fatty acids (and the corresponding number of carbons) found in MCTs are caproic acid (C6), caprylic acid (C8), capric acid (C10) and lauric acid (C12). MCTs are composed of a glycerol backbone and three of these fatty acids. The approximate ratios of these fatty acids in commercial MCT products derived from coconut oil are 2(C6):55(C8):42(C10):1(C12).[1]"
Medium chain triglycerides - Monograph in Alternative Medicine Review (2002)
"Up to 30 percent of MCTs are absorbed intact across the intestinal barrier and directly enter the portal vein. This allows for much quicker absorption and utilization of MCTs compared to LCTs. MCTs are transported into the mitochondria independent of the carnitine shuttle, which is necessary for LCT-mitochondrial absorption. Oxidation of MCTs provides 8.3 calories per gram."
"Medium Chain Triglycerides (MCTs): Beneficial Effects on Energy, Atherosclerosis and Aging" in Nutrition Review
"Partial Replacement of Dietary (n-6) Fatty Acids with Medium-Chain Triglycerides Decreases the Incidence of Spontaneous Colitis in Interleukin-10–Deficient Mice" in The Journal of Nutrition (2009)
" We conclude that partial replacement of dietary (n-6) FA with MCT decreases the incidence of colitis in a model of spontaneous intestinal inflammation and provide experimental arguments for a possible primary therapeutic effect of MCT in human Crohn's disease."
"The vast majority of the fats and oils you eat, whether they are saturated or unsaturated or come from an animal or a plant, are composed of long-chain triglycerides. Probably 98 to 100% of all the fats we eat consist of LCT. Coconut oil is unique because it is composed predominately of MCT. The size of the fatty acid is extremely important because physiological effects of medium-chain fatty acids in coconut oil are distinctly different from the long-chain fatty acids more commonly found in our diet. It's the MCT in coconut oil that make it different from all other fats and for the most part gives it its unique character and healing properties. Almost all of the medium-chain triglycerides used in research, medicine, and food products come from coconut oil."
Medium-chain triglycerides (MCTs)"MCTs passively diffuse from the GI tract to the portal system (longer fatty acids are absorbed into the lymphatic system) without requirement for modification like long-chain fatty acids or very-long-chain fatty acids. In addition, MCTs do not require bile salts for digestion. Patients that have malnutrition or malabsorption syndromes are treated with MCTs because they do not require energy for absorption, utilization, or storage. Coconut oil is composed of approximately 66% medium-chain triglycerides. Other rich sources of MCTs include palm kernel oils and camphor tree drupes. The fatty acids found in MCTs are called medium-chain fatty acids. The names of the medium-chain fatty acids (and the corresponding number of carbons) found in MCTs are caproic acid (C6), caprylic acid (C8), capric acid (C10) and lauric acid (C12). MCTs are composed of a glycerol backbone and three of these fatty acids. The approximate ratios of these fatty acids in commercial MCT products derived from coconut oil are 2(C6):55(C8):42(C10):1(C12).[1]"
Medium chain triglycerides - Monograph in Alternative Medicine Review (2002)
"Up to 30 percent of MCTs are absorbed intact across the intestinal barrier and directly enter the portal vein. This allows for much quicker absorption and utilization of MCTs compared to LCTs. MCTs are transported into the mitochondria independent of the carnitine shuttle, which is necessary for LCT-mitochondrial absorption. Oxidation of MCTs provides 8.3 calories per gram."
"Medium Chain Triglycerides (MCTs): Beneficial Effects on Energy, Atherosclerosis and Aging" in Nutrition Review
"Partial Replacement of Dietary (n-6) Fatty Acids with Medium-Chain Triglycerides Decreases the Incidence of Spontaneous Colitis in Interleukin-10–Deficient Mice" in The Journal of Nutrition (2009)
" We conclude that partial replacement of dietary (n-6) FA with MCT decreases the incidence of colitis in a model of spontaneous intestinal inflammation and provide experimental arguments for a possible primary therapeutic effect of MCT in human Crohn's disease."
Does a low-fat diet reduce Crohn's symptoms?
Low Fat Diet from Wikipedia
"... a diet that consists of little fat, especially saturated fat and cholesterol ..."
"Nutritional and metabolic issues in inflammatory bowel disease" in Curr Opin Clin Nutr Metab Care (2003)
"Low-fat diets, with added amounts of medium-chain triglycerides, are useful in decreasing gut inflammation in the condition. The search for the optimal dietary fatty acid composition deserves further investigations." [emphasis mine]
"... a diet that consists of little fat, especially saturated fat and cholesterol ..."
"Nutritional and metabolic issues in inflammatory bowel disease" in Curr Opin Clin Nutr Metab Care (2003)
"Low-fat diets, with added amounts of medium-chain triglycerides, are useful in decreasing gut inflammation in the condition. The search for the optimal dietary fatty acid composition deserves further investigations." [emphasis mine]
Does a low-carb diet improve Crohn's symptoms?
See Jimmy Moore's Livin' La Vida Low-Carb
See Jacqueline Eberstein's Controlled Carbohydrate Nutrition
Atkins
"Lectins in the United States diet: a survey of lectins in commonly consumed foods and a review of the literature" in Am J Clin Nutr (1980) [full pdf version] [includes food lists]
"Although both cooking and the normal digestive processes might be expected to blunt or abrogate dietary lectin activity, this need not necessarily be the case. ... [D]ry heat may not completely destroy lectin activity .... clearly illustrated in the finding of hemagglutinating activity in the processed wheatgerm, peanuts, and dry cereals that we tested. ... [S]everal of the lectins have been found to be resistant to proteolytic digestion e.g., wheat germ agglutinin, tomato lectin, navy bean lectin and, when looked for, have been recovered intact in stool. ... [S]ome lectins in foodstuffs will survive one or both degradative processes to interact with cells, secretions, and microflora of the digestive tract resulting in, as yet unknown, functional consequences."

"The Dark Side of Wheat" by Sayer Ji on GreenMedInfo.com
"Opening Pandora's Bread Box: The Critical Role of Wheat Lectin in Human Disease" by Sayer Ji, GreenMedInfo.com
See Jacqueline Eberstein's Controlled Carbohydrate Nutrition
Atkins
"Lectins in the United States diet: a survey of lectins in commonly consumed foods and a review of the literature" in Am J Clin Nutr (1980) [full pdf version] [includes food lists]
"Although both cooking and the normal digestive processes might be expected to blunt or abrogate dietary lectin activity, this need not necessarily be the case. ... [D]ry heat may not completely destroy lectin activity .... clearly illustrated in the finding of hemagglutinating activity in the processed wheatgerm, peanuts, and dry cereals that we tested. ... [S]everal of the lectins have been found to be resistant to proteolytic digestion e.g., wheat germ agglutinin, tomato lectin, navy bean lectin and, when looked for, have been recovered intact in stool. ... [S]ome lectins in foodstuffs will survive one or both degradative processes to interact with cells, secretions, and microflora of the digestive tract resulting in, as yet unknown, functional consequences."

"The Dark Side of Wheat" by Sayer Ji on GreenMedInfo.com
"Opening Pandora's Bread Box: The Critical Role of Wheat Lectin in Human Disease" by Sayer Ji, GreenMedInfo.com
20.6.11
Do nightshade-family foods worsen Crohn's symptoms?
Solanaceae at Wikipedia
"What are nightshades and in which foods are they found?" on the world's healthiest foods
"Potatoes, tomatoes, sweet and hot peppers, eggplant, tomatillos, tamarios, pepinos, pimentos, paprika, cayenne, and Tabasco sauce are classified as nightshade foods. A particular group of substances in these foods, called alkaloids, can impact nerve-muscle function and digestive function in animals and humans, and may also be able to compromise joint function. Because the amount of alkaloids is very low in nightshade foods when compared with other nightshade plants, health problems from nightshade foods may only occur in individuals who are especially sensitive to these alkaloid substances. Since cooking only lowers alkaloid content of nightshade foods by about 40-50%, highly sensitive individuals may want to avoid this category of food altogether, while non-sensitive individuals may be able to eat these foods, especially in cooked form, without problem.
"What are nightshades and in which foods are they found?" on the world's healthiest foods
"Potatoes, tomatoes, sweet and hot peppers, eggplant, tomatillos, tamarios, pepinos, pimentos, paprika, cayenne, and Tabasco sauce are classified as nightshade foods. A particular group of substances in these foods, called alkaloids, can impact nerve-muscle function and digestive function in animals and humans, and may also be able to compromise joint function. Because the amount of alkaloids is very low in nightshade foods when compared with other nightshade plants, health problems from nightshade foods may only occur in individuals who are especially sensitive to these alkaloid substances. Since cooking only lowers alkaloid content of nightshade foods by about 40-50%, highly sensitive individuals may want to avoid this category of food altogether, while non-sensitive individuals may be able to eat these foods, especially in cooked form, without problem.
...
Effect of steroid alkaloids on joint health ... Some researchers have speculated that nightshade alkaloids can contribute to excessive loss of calcium from bone and excessive depositing of calcium in soft tissue. For this reason, these researchers have recommended elimination of nightshade foods from the meal plans of all individuals with osteoarthritis, rheumatoid arthritis, or other joint problems like gout.
...
Effect of nicotine alkaloid on health ... While we agree that the amount of nicotine in nightshade foods is very, very small, it still seems possible to us that some individuals might be particularly sensitive to the alkaloids found in nightshades, and that even very small amounts might compromise function in the bodies of these individuals."
18.6.11
Does a paleo diet reduce Crohn's symptoms?
The Paleo Diet and Crohn's Disease on The Paleo Diet
 Read the a dietitian gone paleo blog to get a trained dieticians views on mainstream versus paleo diets as well as gluten-free, legume-free, dairy-free, processed food-free + low-FODMAPs + low in natural food chemicals.
Read the a dietitian gone paleo blog to get a trained dieticians views on mainstream versus paleo diets as well as gluten-free, legume-free, dairy-free, processed food-free + low-FODMAPs + low in natural food chemicals.
Clinical Studies supporting the Paleo diet (rebuttal to US News)
 Read the a dietitian gone paleo blog to get a trained dieticians views on mainstream versus paleo diets as well as gluten-free, legume-free, dairy-free, processed food-free + low-FODMAPs + low in natural food chemicals.
Read the a dietitian gone paleo blog to get a trained dieticians views on mainstream versus paleo diets as well as gluten-free, legume-free, dairy-free, processed food-free + low-FODMAPs + low in natural food chemicals.Clinical Studies supporting the Paleo diet (rebuttal to US News)
14.6.11
Does a low fibre with low residue diet reduce Crohn's symptoms?
Crohn's and Colitis Foundation of America, Diet and Nutrition
"About two thirds of people with small bowel Crohn's disease develop a marked narrowing (or stricture) of the lower small intestine, the ileum. For these patients, a low-fiber with low-residue diet or a special liquid diet may be beneficial in minimizing abdominal pain and other symptoms. This diet minimizes the consumption of foods that add "scrapy" residue to the stool. These include raw fruits, vegetables, and seeds, as well as nuts and corn hulls. The registered dietitian associated with your IBD treatment program can assist you in devising such a diet when appropriate. Often, these dietary adjustments are temporary; the patient follows them until the inflammation that caused the narrowing responds either to medical treatment or to a corrective surgical procedure."
"About two thirds of people with small bowel Crohn's disease develop a marked narrowing (or stricture) of the lower small intestine, the ileum. For these patients, a low-fiber with low-residue diet or a special liquid diet may be beneficial in minimizing abdominal pain and other symptoms. This diet minimizes the consumption of foods that add "scrapy" residue to the stool. These include raw fruits, vegetables, and seeds, as well as nuts and corn hulls. The registered dietitian associated with your IBD treatment program can assist you in devising such a diet when appropriate. Often, these dietary adjustments are temporary; the patient follows them until the inflammation that caused the narrowing responds either to medical treatment or to a corrective surgical procedure."
Which foods are CDers sensitive to?
"Dietary factors in chronic inflammation: Food tolerances and intolerances of a New Zealand Caucasian Crohn's disease population" in Mutation Research/Fundamental and Molecular Mechanisms of Mutagenesis (2010)
"Abstract
Diet is known to play a major role in the symptoms of the inflammatory bowel disease, Crohn's disease (CD). Although no single diet is appropriate to all individuals, most CD patients are aware of foods that provide adverse or beneficial effects. This study seeks to categorise foods in relation to their effects on symptoms of CD, in a New Zealand Caucasian population. Four hundred and forty-six subjects from two different centres in New Zealand were recruited into the study. An extensive dietary questionnaire (257 food items in 15 groups) recorded self-reported dietary tolerances and intolerances. Across each of the food groups, there were statistically significant differences among responses to foods. A two-dimensional graphical summary enabled stratification of foods according to the probability that they will be either beneficial or detrimental. A small number of foods are frequently considered to be beneficial, including white fish, salmon and tuna, gluten-free products, oatmeal, bananas, boiled potatoes, sweet potatoes (kumara), pumpkin, soya milk, goat's milk and yoghurt. Foods that are typically considered detrimental include grapefruit, chilli or chilli sauce, corn and corn products, peanuts, cream, salami, curried foods, cola drinks, high energy drinks, beer, and red wine. For a number of the food items, the same item that was beneficial for one group of subjects was detrimental to others; in particular soya milk, goat's milk, yoghurt, oatmeal, kiwifruit, prunes, apple, broccoli, cauliflower, linseed, pumpkin seed, sunflower seed, ginger and ginger products, beef, lamb, liver, and oily fish. It was not possible to identify a specific group of food items that should be avoided by all CD patients. The wide range of detrimental items suggests that dietary maintenance of remission is likely to be difficult, and to exclude a substantial number of foods. Personalised diets may be especially important to these individuals." [emphases mine]
"Immune sensitization to food, yeast and bacteria in Crohn’s disease" in Alimentary Pharmacology and Therapeutics (2001) [full article]
"The following groups of antigens were utilized:
1 Cereal grain mix (barley, corn, oat, rice, rye and wheat), 1/10 weight for volume.
2 Cabbage group mix (broccoli, brussel sprouts, cabbage and cauliflower), 1/10 weight for volume.
3 Citrus mix (grapefruit, lemon, lime and sweet orange), 1/10 weight for volume.
4 Whole cow’s milk, 1/20 weight for volume.
5 Bakers yeast and brewers yeast (Saccharomyces cerevisiae), 1/10 weight for volume.
6 Peanut mix (runner peanut, Virginia, Spanish), 200 protein nitrogen units/mL. ...
The following positive proliferative responses were noted in Crohn’s disease patients: 13 to milk, 16 to cabbage, 14 to cereal, nine to citrus, 16 to peanut, 18 to E. coli, 11 to Bacteroides, 10 to Klebsiella, six to bakers yeast, and nine to brewers yeast."
"Gut mucosal response to food antigens in Crohn's disease" in Alimentary Pharmacology and Therapeutics (2002) [full article]
"Although the strongest data were obtained for a response to citrus fruit and yeast antigens, the individual data supported the possibility of an abnormal response to the full range of antigen groups tested. In an individual, any one or more of these protein groups may be important." [emphasis mine]
"What Is the Role of Food Allergy and/or Intolerance in the Genesis of IBD?" in General Gastroenterology (2006)
"True food allergies constitute a different pathogenesis and pathology from true IBD. Although the true cause of IBD remains elusive, it appears to involve a combination of genetic susceptibility, immune dysregulation, and environmental pressures. Patients with IBD are more likely to suffer from food allergies or intolerances than the normal population, but there is not good evidence to suggest that an allergy is the trigger for the underlying inflammatory process. Whereas some groups have been able to demonstrate immune responses to certain food antigens in patients with Crohn's disease, these findings cannot be replicated in other populations, making this mechanism for a pathogenesis unlikely. In patients with subclinical disease, an allergy can precipitate IBD phenotypes, but again, the link between allergies and causation is weak. Certainly those patients who have undiagnosed food intolerances are less likely to respond to standard IBD therapies.
Patients should be counseled regarding their dietary habits to monitor which specific foods or food groups may trigger worse gastrointestinal or systemic symptoms. Elimination diets, however, are rarely needed in the IBD patient."
"The role of diet in the management of inflammatory bowel disease" in World J Gastroenterol (2010) "Studies that aim to isolate culpable food groups have shown that individuals react differently on exposure to or exclusion of various foods. The commonly identified food sensitivities are cereals, milk, eggs, vegetables and citrus fruits"
Crohn's and Colitis Foundation of America, Diet and Nutrition
"Do any specific foods worsen the inflammation of IBD?
No. Although certain foods may aggravate symptoms of these diseases, there is no evidence that the inflammation of the intestine is directly affected. Obviously, any contaminated food that leads to food poisoning or dysentery will aggravate IBD. ... Again, there are no blanket rules or recommendations. If a particular kind of food causes digestive problems, then try to avoid it. But it's important to distinguish between an actual allergy to one kind of food and an intolerance. Many people have food intolerances -- far more than really have true food allergies. Elimination tests are better at diagnosing which foods must be avoided or modified than the standard allergy skin or blood testing. Many good books discuss the proper way to follow such an "elimination diet," which involves keeping a food and symptom diary over several weeks."
"Abstract
Diet is known to play a major role in the symptoms of the inflammatory bowel disease, Crohn's disease (CD). Although no single diet is appropriate to all individuals, most CD patients are aware of foods that provide adverse or beneficial effects. This study seeks to categorise foods in relation to their effects on symptoms of CD, in a New Zealand Caucasian population. Four hundred and forty-six subjects from two different centres in New Zealand were recruited into the study. An extensive dietary questionnaire (257 food items in 15 groups) recorded self-reported dietary tolerances and intolerances. Across each of the food groups, there were statistically significant differences among responses to foods. A two-dimensional graphical summary enabled stratification of foods according to the probability that they will be either beneficial or detrimental. A small number of foods are frequently considered to be beneficial, including white fish, salmon and tuna, gluten-free products, oatmeal, bananas, boiled potatoes, sweet potatoes (kumara), pumpkin, soya milk, goat's milk and yoghurt. Foods that are typically considered detrimental include grapefruit, chilli or chilli sauce, corn and corn products, peanuts, cream, salami, curried foods, cola drinks, high energy drinks, beer, and red wine. For a number of the food items, the same item that was beneficial for one group of subjects was detrimental to others; in particular soya milk, goat's milk, yoghurt, oatmeal, kiwifruit, prunes, apple, broccoli, cauliflower, linseed, pumpkin seed, sunflower seed, ginger and ginger products, beef, lamb, liver, and oily fish. It was not possible to identify a specific group of food items that should be avoided by all CD patients. The wide range of detrimental items suggests that dietary maintenance of remission is likely to be difficult, and to exclude a substantial number of foods. Personalised diets may be especially important to these individuals." [emphases mine]
"Immune sensitization to food, yeast and bacteria in Crohn’s disease" in Alimentary Pharmacology and Therapeutics (2001) [full article]
"The following groups of antigens were utilized:
1 Cereal grain mix (barley, corn, oat, rice, rye and wheat), 1/10 weight for volume.
2 Cabbage group mix (broccoli, brussel sprouts, cabbage and cauliflower), 1/10 weight for volume.
3 Citrus mix (grapefruit, lemon, lime and sweet orange), 1/10 weight for volume.
4 Whole cow’s milk, 1/20 weight for volume.
5 Bakers yeast and brewers yeast (Saccharomyces cerevisiae), 1/10 weight for volume.
6 Peanut mix (runner peanut, Virginia, Spanish), 200 protein nitrogen units/mL. ...
The following positive proliferative responses were noted in Crohn’s disease patients: 13 to milk, 16 to cabbage, 14 to cereal, nine to citrus, 16 to peanut, 18 to E. coli, 11 to Bacteroides, 10 to Klebsiella, six to bakers yeast, and nine to brewers yeast."
"Gut mucosal response to food antigens in Crohn's disease" in Alimentary Pharmacology and Therapeutics (2002) [full article]
"Although the strongest data were obtained for a response to citrus fruit and yeast antigens, the individual data supported the possibility of an abnormal response to the full range of antigen groups tested. In an individual, any one or more of these protein groups may be important." [emphasis mine]
"What Is the Role of Food Allergy and/or Intolerance in the Genesis of IBD?" in General Gastroenterology (2006)
"True food allergies constitute a different pathogenesis and pathology from true IBD. Although the true cause of IBD remains elusive, it appears to involve a combination of genetic susceptibility, immune dysregulation, and environmental pressures. Patients with IBD are more likely to suffer from food allergies or intolerances than the normal population, but there is not good evidence to suggest that an allergy is the trigger for the underlying inflammatory process. Whereas some groups have been able to demonstrate immune responses to certain food antigens in patients with Crohn's disease, these findings cannot be replicated in other populations, making this mechanism for a pathogenesis unlikely. In patients with subclinical disease, an allergy can precipitate IBD phenotypes, but again, the link between allergies and causation is weak. Certainly those patients who have undiagnosed food intolerances are less likely to respond to standard IBD therapies.
Patients should be counseled regarding their dietary habits to monitor which specific foods or food groups may trigger worse gastrointestinal or systemic symptoms. Elimination diets, however, are rarely needed in the IBD patient."
"The role of diet in the management of inflammatory bowel disease" in World J Gastroenterol (2010) "Studies that aim to isolate culpable food groups have shown that individuals react differently on exposure to or exclusion of various foods. The commonly identified food sensitivities are cereals, milk, eggs, vegetables and citrus fruits"
Crohn's and Colitis Foundation of America, Diet and Nutrition
"Do any specific foods worsen the inflammation of IBD?
No. Although certain foods may aggravate symptoms of these diseases, there is no evidence that the inflammation of the intestine is directly affected. Obviously, any contaminated food that leads to food poisoning or dysentery will aggravate IBD. ... Again, there are no blanket rules or recommendations. If a particular kind of food causes digestive problems, then try to avoid it. But it's important to distinguish between an actual allergy to one kind of food and an intolerance. Many people have food intolerances -- far more than really have true food allergies. Elimination tests are better at diagnosing which foods must be avoided or modified than the standard allergy skin or blood testing. Many good books discuss the proper way to follow such an "elimination diet," which involves keeping a food and symptom diary over several weeks."
13.6.11
Is anything sweet good for CD?
The Specific Carbohydrate Diet limits sweets to monosaccharides such as honey.
The FODMAP diet limits sweet to glucose predominant foods.
But is any sweet good for CD? Is it possible to give up sweetness?
"Role of diet in the management of inflammatory bowel disease" in World J Gastroenterol (2010)
"Exclusion of sugar shows little evidence of amelioration in CD."
The FODMAP diet limits sweet to glucose predominant foods.
But is any sweet good for CD? Is it possible to give up sweetness?
"Role of diet in the management of inflammatory bowel disease" in World J Gastroenterol (2010)
"Exclusion of sugar shows little evidence of amelioration in CD."
5.6.11
Does avoiding yeast reduce the symptoms of Crohn's?
"Immune sensitization to yeast antigens in ASCA-positive patients with Crohn's disease" in Inflammtory Bowel Disease (2006)
"In summary, mannan antigens play an important role by interacting in different ways with the immune system. The reactivity of the immune system toward mannans seems to be disturbed specifically in patients with CD. Because mannans are ubiquitous, it is difficult to verify their immune modulatory influence. Interestingly, Young et al. reported that the clinical activity of CD could be reduced by avoiding yeast antigens. 13 However, it is doubtful whether a total avoidance of yeast antigens is possible."
"In summary, mannan antigens play an important role by interacting in different ways with the immune system. The reactivity of the immune system toward mannans seems to be disturbed specifically in patients with CD. Because mannans are ubiquitous, it is difficult to verify their immune modulatory influence. Interestingly, Young et al. reported that the clinical activity of CD could be reduced by avoiding yeast antigens. 13 However, it is doubtful whether a total avoidance of yeast antigens is possible."
Does eliminating yeast improve Crohn's symptoms?
Synonyms for yeast:
- leavening (always yeast)
- hydrolysed protein (usually yeast)
- hydrolysed vegetable protein (usually yeast)
Does an IgG4-targeted exclusion diet improve CD symptoms?
About IgG4 antibody-mediated immunity
Metametrix's Allergix IgG4 Antibodies 90 - serum
"IgG4 antibodies are associated with non-atopic or "delayed" food reactions...."
Common offending foods: milk, corn, wheat, eggs, foods processed with moulds (black teas, breads, fruit juices)
Also see Downloads section (bottom right) for Allergix Antibody Profiles, IgG4 Food Antibody Interpretation
"Anti-Inflammatory Activity of Human IgG4 Antibodies by Dynamic Fab Arm Exchange" in Science (2007)
Conclusions: "In summary, antibodies of the IgG4 isotype are shown to be dynamic molecules, undergoing Fab arm exchange in vivo and in vitro. The ability to engage in Fab arm exchange appears to be an inherent feature of IgG4 that involves the third constant domain in addition to the hinge region and that only requires a reducing environment to be activated. This novel protein modification challenges the commonly accepted one antibody–one antigen paradigm and redefines our thinking about the role of IgG4 in antibody-mediated immunity and the application of IgG4 monoclonal antibodies to immunotherapy."
IgG4 in IBS
"Food-specific IgG4 antibody-guided exclusion diet improves symptoms and rectal compliance in irritable bowel syndrome." in Scand J Gasterol (2005)
Results: "IgG4 antibodies to milk, eggs, wheat, beef, pork and lamb were commonly elevated."
Conclusions: "Food-specific IgG4 antibody-guided exclusion diet improves symptoms in IBS and is associated with an improvement in rectal compliance."
IgG4 in CD
"Food specific IgG4 -guided exclusion diets improve symptoms in Crohn’s disease: A pilot study" in Colorectal Disease (2010)
Conclusions: "IgG4-guided exclusion diets resulted in significant symptomatic improvement with an objective fall in an inflammatory marker. This approach may be useful in clinical practice."
"Clinical Relevance of IgG Antibodies against Food Antigens in Crohn’s Disease: A Double-Blind Cross-Over Diet Intervention Study" in Digestion (2010)
Conclusions: "A nutritional intervention based on circulating IgG antibodies against food antigens showed effects with respect to stool frequency. The mechanisms by which IgG antibodies might contribute to disease activity remain to be elucidated."
Metametrix's Allergix IgG4 Antibodies 90 - serum
"IgG4 antibodies are associated with non-atopic or "delayed" food reactions...."
Common offending foods: milk, corn, wheat, eggs, foods processed with moulds (black teas, breads, fruit juices)
Also see Downloads section (bottom right) for Allergix Antibody Profiles, IgG4 Food Antibody Interpretation
"Anti-Inflammatory Activity of Human IgG4 Antibodies by Dynamic Fab Arm Exchange" in Science (2007)
Conclusions: "In summary, antibodies of the IgG4 isotype are shown to be dynamic molecules, undergoing Fab arm exchange in vivo and in vitro. The ability to engage in Fab arm exchange appears to be an inherent feature of IgG4 that involves the third constant domain in addition to the hinge region and that only requires a reducing environment to be activated. This novel protein modification challenges the commonly accepted one antibody–one antigen paradigm and redefines our thinking about the role of IgG4 in antibody-mediated immunity and the application of IgG4 monoclonal antibodies to immunotherapy."
IgG4 in IBS
"Food-specific IgG4 antibody-guided exclusion diet improves symptoms and rectal compliance in irritable bowel syndrome." in Scand J Gasterol (2005)
Results: "IgG4 antibodies to milk, eggs, wheat, beef, pork and lamb were commonly elevated."
Conclusions: "Food-specific IgG4 antibody-guided exclusion diet improves symptoms in IBS and is associated with an improvement in rectal compliance."
IgG4 in CD
"Food specific IgG4 -guided exclusion diets improve symptoms in Crohn’s disease: A pilot study" in Colorectal Disease (2010)
Conclusions: "IgG4-guided exclusion diets resulted in significant symptomatic improvement with an objective fall in an inflammatory marker. This approach may be useful in clinical practice."
"Clinical Relevance of IgG Antibodies against Food Antigens in Crohn’s Disease: A Double-Blind Cross-Over Diet Intervention Study" in Digestion (2010)
Conclusions: "A nutritional intervention based on circulating IgG antibodies against food antigens showed effects with respect to stool frequency. The mechanisms by which IgG antibodies might contribute to disease activity remain to be elucidated."
Subscribe to:
Posts (Atom)